NORFOLK, Va. — It's the long-awaited light at the end of the tunnel: the sight of shots going into people's arms and COVID-19 case counts falling, But our "new normal" has perhaps masked the dark underbelly of what the pandemic revealed about the healthcare system in the United States.
"You look at how we responded to the pandemic, arguably the worst of any country in the world," said Dr. William Oldfield, an infectious disease expert at EVMS who argues our healthcare system wasn't prepared for COVID-19.
During the 2009 swine flu outbreak, the Strategic National Stockpile distributed 85 million masks, gloves, and gowns. None of that was replaced. Instead, a decision was made to stockpile medicines developed to deal with the threat of a bio-terrorist attack.
Additionally, the U.S. saw an 18 percent drop in public health funding and the loss of 38,000 jobs.
"So we entered this pandemic with a completely depleted and underfunded public health system," Dr. Oldfield said.
Dr. Patrick Jackson, an infectious disease expert with UVA Health, sees gaps in the delivery of healthcare as well.
"In reality, we spend a huge amount of money on healthcare, but we don't spend nearly enough on public health or infectious research, especially on infectious diseases," Jackson said, adding COVID-19 revealed a lack of effective public health infrastructure to get people to wear masks and social distance.
He also feels some physicians struggled to understand and integrate the new research and data that came out of COVID-19.
"The use of hydroxychloroquine early on didn't pan out well, and we should have recognized that sooner than we did," Jackson said.
While there have been long-standing inequities in our healthcare system, many feel the pandemic made them worse.
"If you look on the forefront of COVID-19, Black and Brown people were sent home and told they were not sick enough," said Gaylene Kanoyton, a healthcare and political consultant, adding it wasn't until deaths started climbing that the healthcare system better focused on inequities.
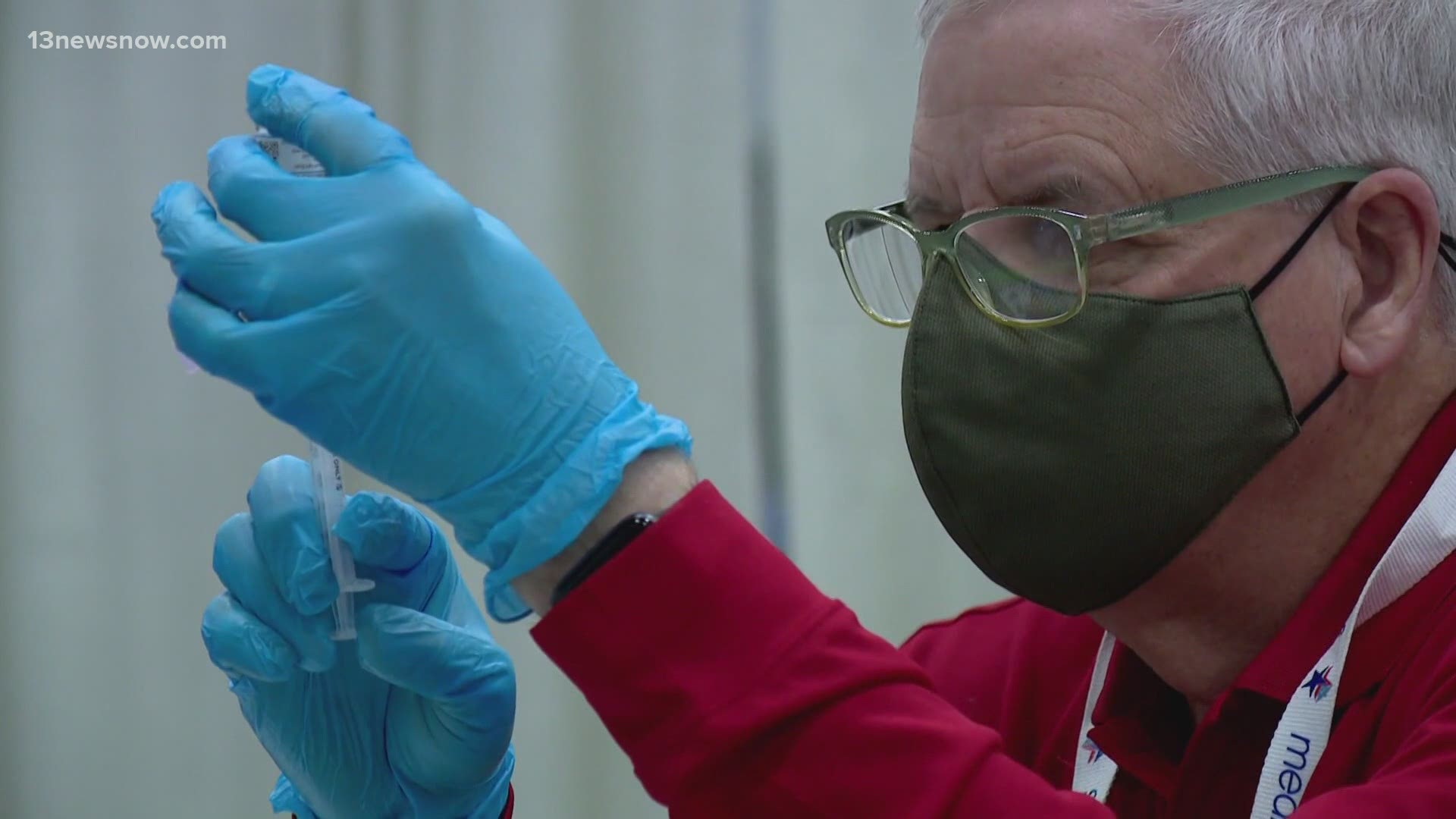
On the positive side, COVID-19 also revealed strength and resilience in our healthcare system. We saw the bravery of frontline healthcare workers. More people had access to regular medical exams with the ACA and with Medicaid expansion in the Commonwealth, and three very effective vaccines were developed very quickly.
"If you would have told me in the spring what the chance was of having a vaccine 95% effective by the end of the year, I would have said, 'Absolutely incredible,'" Dr. Oldfield said.
Medical experts say many of us will see another pandemic in our lifetimes, maybe two. We'll need a healthcare system better focused on handling a surge, greater investment in biomedical research, better sharing of data, and the need to keep politics out of pandemics.
Finally, is the fear we've felt for the last year, and the loved ones we've lost, enough to summon the courage to reboot, reimagine and re-examine our healthcare system? Is it a debate we're willing to have?
Dr. Jackson added, "If you have a choice between spending trillions on a new fighter jet or investing more in the National Institutes of Health to turn out vaccines quicker, I think there's an argument that needs to be made for the latter."